Once babies are a year old, those who have been drinking infant formula don’t need it anymore. By that age, they can and should get most of their nutritional needs met by solid foods. Drinking cow’s milk, or a fortified plant milk such as soy milk, is perfectly fine. And honestly, they don’t even need that much of it.
A 2023 report from the American Academy of Pediatrics (AAP) looked closely at what toddlers actually need for healthy growth and development — and toddler milks didn’t make the cut. Here are a few key takeaways for parents.
Is toddler formula more nutritious than milk?
No. But for some parents, it feels odd and uncomfortable to stop formula and give cow’s milk. They feel like formula is more nutritious and maybe even more easily digested. That may not be surprising: a lot of marketing money has encouraged people to think this way.
So it’s understandable that some parents turn to formulas marketed for toddlers. It’s especially understandable given the claims that formula companies make about the nutritional advantages of toddler formula. You may have seen — or bought — these products marketed purely as “follow-up formulas,” “transition formulas,” or “growing-up milks.” These formulas do not have a medical purpose. They simply help companies keep the customers they would otherwise lose once babies turn a year old.
Not only are toddler formulas unnecessary, some of them are actually worse than cow’s milk. That’s the main message shared by the AAP, which hopes to help parents understand what older infants and toddlers actually need — and see through the marketing claims.
Do some toddlers need specialized formulas?
Yes. Just to be clear, I am not talking about specialized formulas for children over 12 months who have digestive, metabolic, or other medical problems.
Are toddler formulas regulated in any way?
No. Because infant formulas must meet all the nutritional requirements of babies less than 12 months of age, they are regulated by the FDA. The FDA has requirements about what they must and must not contain, and it makes sure that the facilities where infant formulas are made are regularly inspected.
This is not true of toddler formulas. They are not regulated, and not required to prove any of the claims they make about their nutritional benefits.
What might make a toddler formula unhealthy?
Given the lack of regulation, it’s not surprising that there is wide variation in the composition of toddler formulas. But what is particularly worrisome, says the AAP, is that some of these products are actually unhealthy. They may have too little or too much protein, or have added sweeteners. These added sweeteners can build a child’s “sweet tooth” and set them on the path to obesity.
Additionally, toddler formulas are more expensive than cow’s milk, creating a financial burden for families — one that is definitely not worth it.
Is your toddler’s diet healthy?
Instead of reaching for a toddler formula, try to take a broader look at your child’s diet. Toddlers should eat from the same healthy food groups we all need. This includes
- fruits and vegetables
- whole grains
- protein (such as meat, fish, beans, and nut butters)
- dairy or dairy substitutes fortified with calcium and vitamin D.
Limit added sugars, and after age 2 try to limit less-healthy fats in the child’s diet as well. The best way to build healthy lifetime habits is to start early, and this is particularly true of nutrition.
About the Author

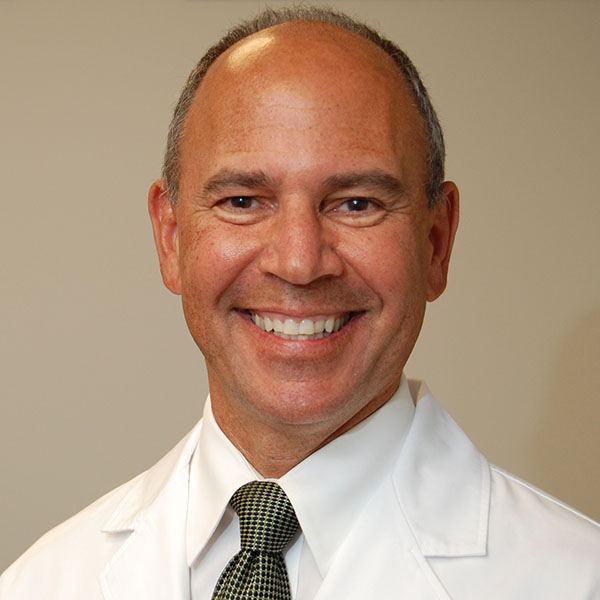
Claire McCarthy, MD, Senior Faculty Editor, Harvard Health Publishing
Claire McCarthy, MD, is a primary care pediatrician at Boston Children’s Hospital, and an assistant professor of pediatrics at Harvard Medical School. In addition to being a senior faculty editor for Harvard Health Publishing, Dr. McCarthy … See Full Bio View all posts by Claire McCarthy, MD